Covered Services
Update your TRICARE eligibility status. To update eligibility status for a family member, contact the Defense Enrollment Eligibility Reporting System (DEERS) at (800) 538-9552 and verify what documentation is required for the change. It is the responsibility of the TRICARE beneficiary, parent or legal representative to report a change in status. Copayments are per occurrence or per visit. Cost-shares are a percentage of the contracted rate for network providers and the maximum TRICARE allowable for non-network providers on certain types of services. Beneficiaries have an out-of-pocket maximum for covered medical expenses; this is known as the catastrophic cap.
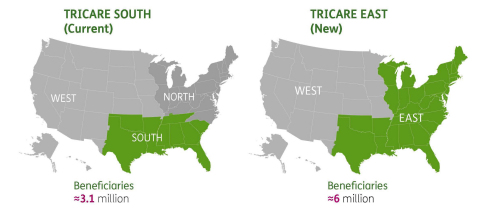
The TRICARE Pharmacy Program, administered by Express Scripts, is designed to provide the medications beneficiaries need, when they need them, in a safe, convenient and cost-effective manner. TRICARE East Region Online Claims Submissions. Qualified TRICARE East Region providers can enter claims into the portal for transmission to WPS and view remittance advices. To submit TRICARE East Region claims on the Humana Military secured provider portal, you must be enrolled in Humana Military(go to Provider Resources Self-Service). TRICARE East providers get information on referrals, eligibility, claims and more.
Learn more about what we cover -including health, dental, and pharmacy.
Mental health problems can affect your thoughts, mood and behavior.
- If you or a family member needs help, call a crisis hotline now!
- If you're not sure, call the Nurse Advice Line.
Learn about TRICARE's mental health coverage.
Several telehealth services are available to TRICARE beneficiaries seeking mental health and substance use disorders treatments.
Some of these services include: Intensive Outpatient Programs, Medication Assisted Treatment, Opioid Treatment Programs, psychotherapy, crisis management, family therapy, group therapy, medication management, and occupational therapy. >> Learn more
Last Updated 5/17/2019
Tricare North Copays
Find a Doctor
Mental Health and Substance Use Disorder Fact Sheet
Costs
 Find your TRICARE costs, including copayments,
Find your TRICARE costs, including copayments,enrollment fees, and payment options.
- Most costs are for calendar year 2021 unless noted separately.
- For US Family Health Plan and TRICARE Prime Remote costs, choose 'TRICARE Prime' from the pull-down menu
- Visit the Cost Terms page for definitions to help you better understand TRICARE costs.
- If you're an unremarried former spouse, for the Continued Health Care Benefit Program (CHCBP), chose 'Retired' regardless of your sponsor's status
- Looking for dental costs? Visit the TRICARE Dental Costs section.
Tricare East Copay For Physical Therapy
Copayments will be waived retroactively to March 18 for certain testing and office visits related to the testing. The test must be one approved, cleared, or authorized by the Food and Drug Administration to detect SARS-CoV-2 or diagnose COVID-19. If you paid any copayments for testing related to COVID-19 and the resulting office visits with a network or non- network provider, you may file a claim for reimbursement. For more information related to the coronavirus, visit the FAQ page.
